Abstract
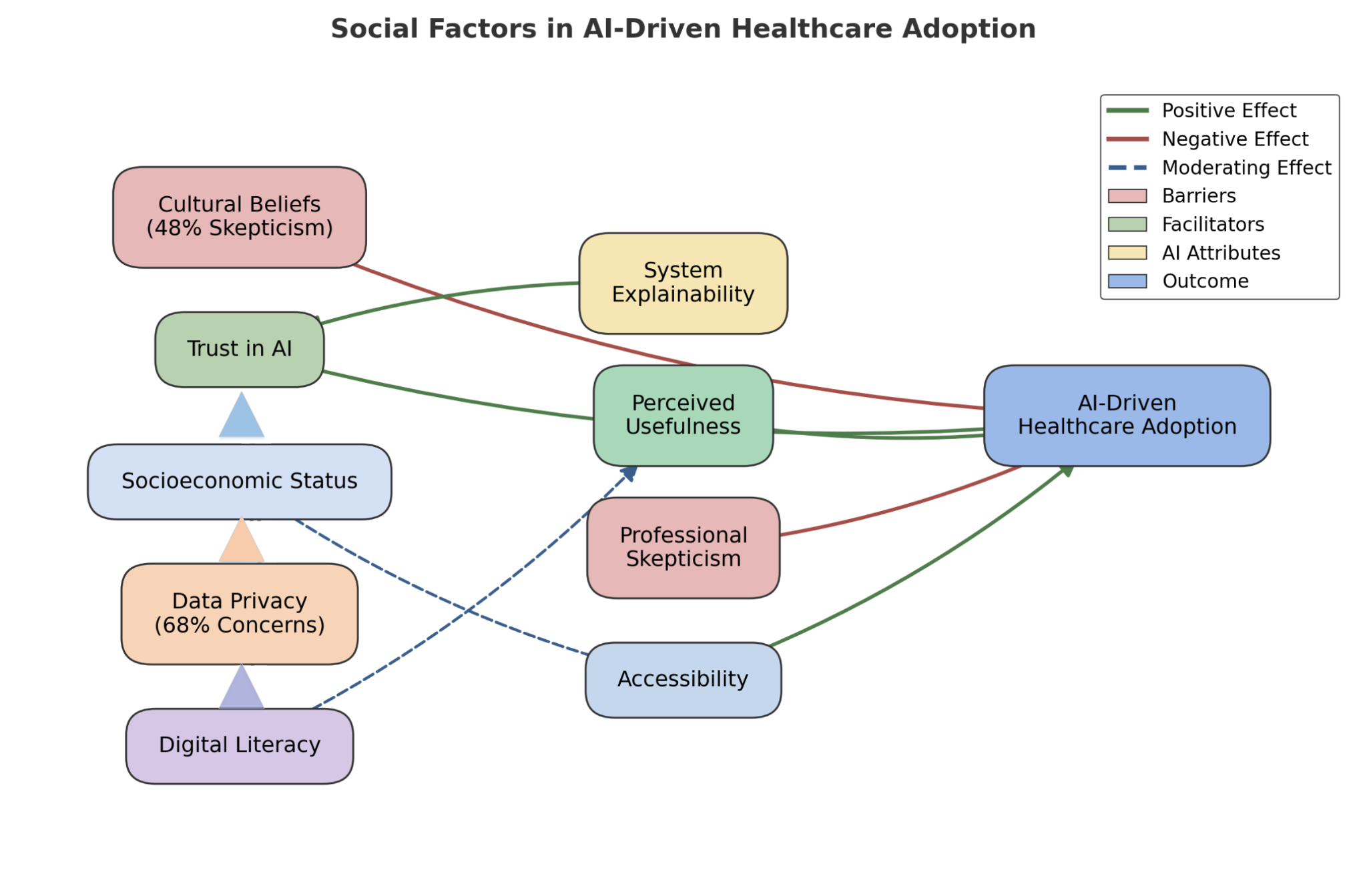
Artificial intelligence (AI) is transforming personalized medicine through its potential. However, implementing AI-driven healthcare solutions remains inconsistent because of certain social factors, i.e., cultural beliefs, trust issues, and major accessibility elements. This study focuses on the key social determinants involved in the acceptance and implementation of AI-driven medicine, with a prime focus on hurdles such as algorithmic bias, transparency issues, and public skepticism. A quantitative approach was employed in the research, and survey data were collected among healthcare professionals, policymakers, and patients. Statistical analyses were performed, including chi-square tests and multiple regression modeling. It examined relationships between social factors and AI adoption rates. The findings presented that familiarity with AI positively influences its acceptance However, the concerns about non-transparent algorithms and cultural resistance continue to hinder its adoption. Nearly 48% of respondents exhibited low attitudes toward AI-driven healthcare. On the other hand, 68% showed concerns about data security. Furthermore, socioeconomic disparities impact accessibility to a great extent, with lower-income groups reporting limited exposure to AI-powered medical solutions. The study also identified transparency as both a facilitator and a barrier, with clinicians hesitant to rely on AI systems due to the lack of explainability. Addressing all these barriers through targeted education, trust-building initiatives, and ethical oversight can increase the equitable integration of AI-driven personalized medicine in diverse settings of healthcare settings.
Data Availability Statement
Data will be made available on request.
Funding
This work was supported without any funding.
Conflicts of Interest
Fiza Aslam and Muhammad Aftab Ur Rehman are employees of Cybex IT Group, Faisalabad 38000, Pakistan.
Ethical Approval and Consent to Participate
Not applicable.
Cite This Article
APA Style
Nadeem, M., Aslam, F., Rehman, M. A. U., & Aslam, S. (2025). Role of Social Factors in the Adoption of AI-Driven Personalized Healthcare. Journal of Artificial Intelligence in Bioinformatics, 1(1), 30–40. https://doi.org/10.62762/JAIB.2025.345522
Publisher's Note
ICCK stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and Permissions
Copyright © 2025 by the Author(s). Published by Institute of Central Computation and Knowledge. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (
https://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.


 Submit Manuscript
Edit a Special Issue
Submit Manuscript
Edit a Special Issue
 Copyright © 2025 by the Author(s). Published by Institute of Central Computation and Knowledge. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
Copyright © 2025 by the Author(s). Published by Institute of Central Computation and Knowledge. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. 